As printed in Michigan Health & Hospitals Magazine, Mar/Apr 1999
THE COMMUNITY BENEFITS COLUMN
Taking Charge of Uncompensated Care, Part II
BY ROBERT M. SIGMOND
Of the billions of dollars that voluntary and government hospitals save because they don't pay most taxes, very little goes into community benefit programs. Rather, this money pays for the increasing volume of uncompensated patient care.
As suggested in my last column (Jan./Feb. 1999), a program to take charge of uncompensated care has great potential to reduce this necessary diversion.
Operated as a collaborative community venture, such a program could open the door for massive funding of improvement in the health status and health systems of the nation's communities.
Those responsible for community benefits can learn from Great Depression experiences, when uncompensated care threatened hospital bankruptcy throughout the land. Although experts were sure that hospitalization was not insurable, hospitals joined in community collaboration to enable people to pay for care on a capitation basis. Identified by the Blue Cross symbol controlled by the American Hospital Association, these early community plans set monthly premiums as low as 50 cents. This was possible because hospitals guaranteed to provide care, whether or not the plan had enough money for reimbursement. The hospitals understood that any payment was better than nothing, since they were going to serve these patients anyway. As these plans grew rapidly, and even attracted commercial insurance competition, the volume of uncompensated care was greatly reduced, freeing up money for expansion of facilities and services. A collaborative community approach saved the day and revolutionized health care financing.
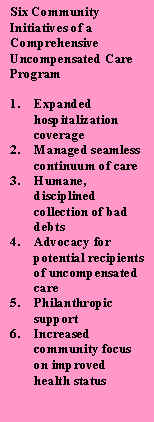
Now that Blue Cross is more concerned with marketplace competition than with uncompensated care, the time has come for hospitals and health systems once more to attack uncompensated care on a community basis. This time, they have the opportunity to renew their commitment to hospitalization coverage within a much broader context. They have everything to gain and little to lose from a successful sixpoint community program to take charge of uncompensated care. (See sidebar.)
In a previous column, I outlined some approaches to assure that uncompensated care patients would have future coverage, even when not able to pay premiums in full or in part. This column will explore two other community initiatives to contain the cost of uncompensated care: managed care and managed collections.
 MANAGED CARE
MANAGED CARE
As currently reflected in the literature, managed care is the responsibility of HMOs and other financing agencies in administering benefits, with little attention to managing care of patients without insurance coverage or other financial resources. Quite frequently, uninsured patients who do not pay are served by different physicians on an episodic basis, without accountable case management. Often, there is no care plan that reflects a seamless continuum, avoidance of duplicative services, effective monitoring of patient compliance, or early detection of complications. Chart reviews reveal many opportunities for significant monetary savings as well as improvement in quality of patient care and patient satisfaction.
A community approach can help each participating hospital achieve more effective management of the care of patients and can monitor and support these efforts while the patient is in the hospital, as well as before and after any hospitalization. Such managed care would involve not only the hospital's clinical care givers, but also other professionals and community activists from a variety of community organizations committed to maintaining a seamless continuum of care.
MANAGED COLLECTIONS
Uncompensated care patients fall into two categories: charity and bad debts. Most studies reveal that the majority of uncompensated care is classified as bad debts rather than charity, probably reflecting significant misclassification. A collaborative, humane two-step approach to bad debt collection should greatly reduce this drain on resources available for community benefit.
The first step in reducing bad debts is a systematic procedure for distinguishing between deserving charity patients and potential deadbeats. Remember the accounting definition of a bad debt. Bad debts are not debts that are uncollectible, as many hospital executives believe. Rather, they are debts that can be collected, but at an estimated cost greater than the amount likely to be collected.
Patients with collection problems should be classified as charity cases as soon as it is clear that the patient's unpaid bill exceeds the amount payable within the family's income and assets, in accordance with established humane, community standards. Such patients should also be classified as social service cases, so that assistance can be provided in financial management and other related family problems. In many cases, this will build a relationship that can result in philanthropic support as well as involvement of the family in an insurance program.
The second step is that all other patients with collection problems should be dealt with humanely but firmly, especially if it appears that the organization may be coping with a potential deadbeat. With a public commitment to serve all, irrespective of inability to pay, the community will support a collection program that is known to pursue all deadbeats into small claims court and beyond. Bad debt write-offs should be extremely rare as contrasted with charity write-offs, even on cases in which the collection costs exceed the estimated payment. Most collection problems of non-urgent admissions can be eliminated by arrangements worked out prior to admission.
ROBERT M. SIGMOND IS A SCHOLAR-IN-RESIDENCE AT THE DEPARTMENT OF HEALTH ADMINISTRATION AT TEMPLE UNIVERSITY, PHILADELPHIA, AND SPECIAL ADVISOR TO THE HEALTH RESEARCH AND EDUCATIONAL TRUST AT THE AMERICAN HOSPITAL ASSOCIATION.
07/06/2000