As printed in Michigan Health & Hospitals Magazine, Jan/Feb 1999
THE COMMUNITY BENEFITS COLUMN
A Community Approach to Managing Uncompensated Care
BY ROBERT M. SIGMOND
Estimated at more than $15 billion annually, uncompensated care accounts for most of the community benefit costs reported by the nation's hospitals. Reflecting the most basic of all hospital goals, these expenditures are designed primarily to benefit patients rather than communities.
In my last column (Nov/Dec 1998), I promised to explore practical ways that communities and hospitals can take charge of uncompensated care to improve patient care outcomes as well as to reduce the financial burden on hospitals and paying patients. Such an approach can also enable hospitals to provide greater community benefits beyond the enhanced benefits to the individual patients.
The timeliness of this topic has been underlined as universal entitlement has again receded into the hazy future while the number of uninsured and inadequately insured is rising. Hospital and health system leaders may be ready to explore the feasibility of a four-step community solution to this problem.
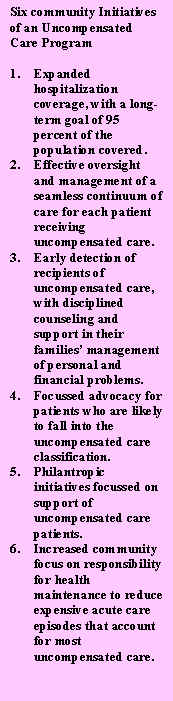 Step One: Design a comprehensive community-based program for managing six specific initiatives that can substantially reduce, and in the long run, virtually eliminate the community's need for uncompensated care.
Step One: Design a comprehensive community-based program for managing six specific initiatives that can substantially reduce, and in the long run, virtually eliminate the community's need for uncompensated care.
Step Two: Create a new profit-making community organization to carry out the program. This new organization would be owned in whole or in part by the area's hospitals, with a broadly representative and accountable community board of directors. The initial goal would be a profit margin of 25 percent by the end of the first year.
Step Three: For support of the new venture, the participating hospitals agree to contribute money equal to their budget lines for uncompensated care and other relevant resources that can be transferred to the new community corporation. The new organization pays the hospitals for all uncompensated care, coordinates/oversees the hospitals' management of uncompensated care patients, and shares the resulting profits with the hospital owners. The hospitals commit to using the profits for expansion of community benefits and for community care network development. Initially, the major expenditure of the new organization would be payments to the hospitals for all uncompensated care, but this would be expected to decline substantially as the program succeeds.
Step Four: If the profit margin is less than 25 percent, a tough management audit would be initiated to determine what went wrong, leading to immediate corrective action within the community organization or at the hospitals.
The key first step is the design of an acceptable, comprehensive program for managing uncompensated care, consisting of at least six major initiatives to be carried out in close collaboration with the hospitals, physicians, and many related community organizations (See sidebar).
Theoretically, each of these six initiatives could be carried out by the hospital alone, but not efficiently enough to justify the effort. The remainder of this column will outline some of the key elements of just the first of the six major initiatives: expansion of hospitalization coverage.
Initially, this initiative involves intensive organized efforts to enroll the family of every individual receiving uncompensated care in a program covering current or future hospital utilization. A case-by-case approach can include systematic steps to assure that such patients are taking advantage of all entitlement programs. At the time when care is being provided, a family is most open to the value of coverage, but these families are not marketed because of their projected heavy loss ratios. But these loss ratios are the very reason the hospitals and community leaders should develop enrollment initiatives; nothing to lose and everything to gain.
Beyond enrolling families of patients, this initiative would involve a series of activities to identify and encourage enrollment of every individual and family who are potential recipients of uncompensated care. This includes the hospital serving as a model for other employers, including broad benefits, choice of plans, and participation in payment of premiums of part-time as well as full-time staff, etc. Related activities include assistance to individuals in forming groups eligible for group premium rates, assistance to individuals in signing up for individual and family coverage outside of groups, and assistance in maintaining coverage following lay-offs, etc. The American Hospital Association's Campaign for Coverage is pioneering this approach, with special attention to children.
A future column will explore the many explicit possibilities for community enrollment of families of potential or active consumers of uncompensated care. For example, an interest-free loan fund might be created to assist such families in payment of their premiums during periods of economic stress such as hospitalization, unemployment, etc. Based on well-known loss ratios of these families, the resulting savings could be significant, even if the rate of loan repayment is not close to 100 percent.
Other columns will explore the other five initiatives in a comprehensive community-based uncompensated care program. Impatient or skeptical readers can contact me at (215) 561-5730 for previews and more details. I would especially welcome calls from individuals with successful or unsuccessful experiences in managing the uncompensated care problem. Although I have set out a rather specific approach to stimulate discussion and action, clearly there is no one right way to proceed on this or any other community-based initiative.
ROBERT M. SIGMOND IS A SCHOLAR-IN-RESIDENCE AT THE DEPARTMENT OF HEALTH ADMINISTRATION AT TEMPLE UNIVERSITY, PHILADELPHIA, AND SPECIAL ADVISOR TO THE HEALTH RESEARCH AND EDUCATIONAL TRUST AT THE AMERICAN HOSPITAL ASSOCIATION.
07/06/2000